Abstract

Purpose
It is difficult to decide whether children with leukemia who could not achieve complete remission (CR) after relapse or primary induction failure should undergo transplantation. Nonetheless, allogeneic hematopoietic stem cell transplantation (HSCT) is a possible approach for refractory acute leukemia including acute lymphoblastic leukemia (ALL). Even after refractory to conventional chemotherapy, a graft versus leukemia (GVL) effect could be expected to some extent. This approach is considered to be experimental because the mortality rate of HSCT is extremely high. A previously conducted large-scale study showed that age younger than 10 years was a factor of good prognosis; however, the details in children are unclear. The purpose of this retrospective analysis was to describe the outcomes and risk factors of HSCT for children with refractory ALL.
Patients and Methods
The data was collected through the Transplant Registry Unified Management Program (TRUMP) system, the registry of The Japan Society for Hematopoietic Cell Transplantation. In total, 325 patients with ALL younger than 21 years old when HSCT was performed between January 2001 and December 2015 and who harbored blasts in peripheral blood and/or bone marrow were analyzed. Both myeloablative regimens and reduced-intensity conditioning regimens were analyzed. Patients were classified as having poor-risk cytogenetics with either t(4;11), t(9;22), t(8;14), hypodiploidy or near triploidy, or more than 5 cytogenetic abnormalities. Other ALL cytogenetic findings were classified as other abnormalities or normal. Myeloablative conditioning was defined as total body irradiation (TBI) of >8 Gy and the administration of 8 mg/kg of busulfan (BU), >140 mg/m2 of melphalan, or >10 mg/kg of thiotepa. All other regimens were analyzed as reduced-intensity conditioning HSCT, including low-dose TBI (≤8 Gy) and low-dose BU (≤8 mg/kg). The graft included bone marrow, peripheral blood stem cells, or cord blood. Overall survival (OS) was used as a primary outcome because for HSCT during relapse, post-HSCT CR was not always achieved or reliably documented.
Results
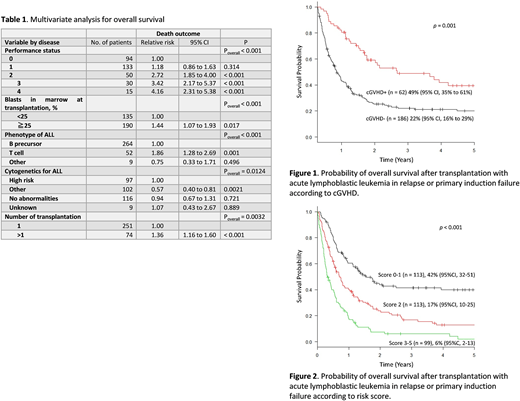
The median follow-up time of survivors was 1145 days (range 110-3710). The median age was 11 years. Thirty-five percent of patients had a pre-HSCT performance status (PS) of 0, which corresponds to a Karnofsky PS of ≥90. The rate of pre-HSCT fungal infection was 14%. Fifty-nine patients had more than 25% marrow blasts when HSCT was performed. When HSCT was performed, 10%, 60%, and 30% of patients exhibited primary induction failure, first relapse, and second or later relapse, respectively. Ninety-one percent of patients had neutrophils and 67% exhibited platelet recovery by day 100. The cumulative incidence of grade II-IV acute graft-versus-host disease (aGVHD) on day 100 was 43%. The cumulative incidence of chronic GVHD (cGVHD) at 3 years after HSCT was 19%. Two hundred and forty-seven patients died. The causes of death were leukemia progression (57%), followed by graft failure (11%), GVHD (10%), hemorrhage (6%), and infection (5%). The 3-year OS rate in all the patients was 22% (95% confidence interval (CI), 18-27). Age, white blood cell count at diagnosis, prior history of central nervous disease, disease status, conditioning regimens, donor-recipient human leukocyte antigen match, graft type, or year in which HSCT was performed did not affect the OS. Grade ≥2 aGVHD did not affect OS. Whereas Patients with chronic GVHD had better 3-year OS (49%, 95% CI 35-61%) compared to that in patients without chronic GVHD (22%, 95% CI 16-29%) (p = 0.001) (Figure 1). Multivariate analysis showed that other than cGVHD, low PS (relative risk (RR): 2.53), blasts in bone marrow greater than 25% (RR: 1.43), T cell phenotype (RR: 1.86), high-risk or normal cytogenetics (RR: 1.42), and a history of HSCT (RR: 1.90) were significant adverse pre-HSCT variables (Table 1). Patients who had 0 or 1 (n = 113), 2 (n = 113), and 3-5 pre-HSCT variables (n = 99) had 42% (95% CI, 32-51), 17% (95% CI, 10-25), and 6% (95% CI, 2-13) 3-year OS, respectively (Figure 2).
Conclusion
Some patients with refractory pediatric ALL achieved relatively long survival following HSCT in the relapsed period, especially when a GVL effect was obtained. A scoring system using pre-HSCT variables should help decide whether HSCT should be performed or not. HSCT is worth considering for children who have undergone ≤2 pre-HSCTs.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal